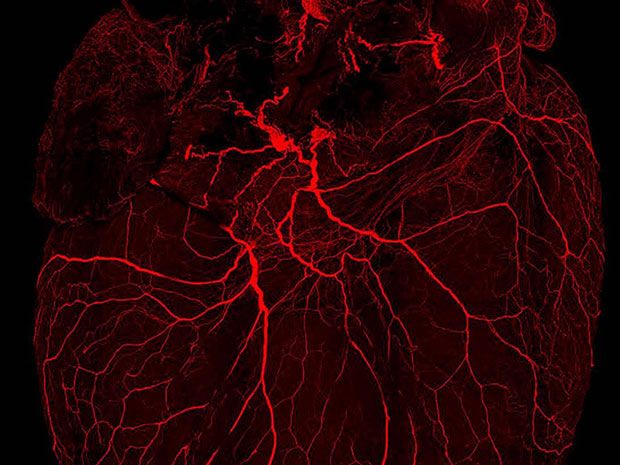
Image: Pradeep Rajendran and Rosemary Challis/Shivkumar Lab/UCLA
The U.S. National Institutes of Health (NIH) wants better ways to treat disease with electrical stimulation, and last week announced the recipients of more than US $20 million in funding for the field. The awards aim to improve maps of the peripheral nervous system—the body’s electrical wiring—and generate sophisticated systems that can hack into its codes.
The funding is part of a $248 million, seven-year program that the NIH Common Fund announced in 2014. Last week’s awards mark the start of the core of that program. Up to $39 million in additional awards will be announced next year. The agency will begin accepting applications for those awards by early 2017, says NIH’s Gene Civillico, who heads up the funding program, called SPARC, or Stimulating Peripheral Activity to Relieve Conditions.
Researchers have for decades been electrically stimulating the brain, the spinal cord and peripheral nerves in an attempt to alleviate ailments such as Parkinson’s disease, epilepsy, pain, and paralysis. The technique can work as well or better than drugs, leading some to dub the field “electroceuticals.” Several companies sell such devices with approval from the U.S. Food and Drug Administration (FDA).
Those tools have seen some success. In clinical studies they have been shown to reduce seizures and symptoms of rheumatoid arthritis, and help people regain bladder control and muscle mobility.
The tools on the market are surprisingly simplistic. In most systems, a pulse generator blindly sends electrical impulses along a lead to electrodes that are placed on a nerve. With enough intensity, the stimulation causes neurons to fire. Those induced impulses, called action potentials, are just like the ones produced naturally by the body. The signals travel along neural networks in different temporal patterns, communicating with the body and influencing chemical and biological processes.
The problem with current devices is that they shoot electrical impulses broadly at nerves in patterns that don’t begin to mimic the body’s natural code. It’s miraculous that the body responds at all to these crude signal patterns. And often the devices activate entire nerves, rather a subset of particular fiber groups, wasting battery power and creating side effects.
That leaves a lot of room for improvement—an exciting prospect for engineers. Many more diseases could be treated with electrical stimulation if the devices were designed more elegantly, say leaders in the field. New designs for electrodes and other tools must better interface with the body and activate nerves that are currently out of reach. And such tools must selectively activate key fibers within the nerve that perform specific functions, these leaders say.
To do that, we need a better understanding of the anatomy of neural circuits—where they are and what they do. We also need to know the precise signal patterns neural circuits use to communicate with organs. In other words, if we want to hack the system, we need maps and codes.
Those are the kinds of breakthroughs NIH Common Fund intends to stimulate with the awards. “We’re seeing a fair bit of clinical success, but with fairly primitive understanding of what the stimulation is actually doing,” says Civillico.
The awards focus on treating conditions such as heart disease, asthma and gastrointestinal disorders. The program’s leaders want researchers to focus on peripheral nerves—those that connect the brain and spinal cord with the rest of the body—because of their potential direct effects on organ systems and their accessibility. (The brain is far more complex, and harder to map.)
