Article in The Pharmaceutical Journal, 9 DEC 2016, By Emma Dorey.
Bioelectronic medicine is a new approach to treating major chronic diseases that could give doctors and patients alternatives to costly mainstream medicine and may become as commonly prescribed as chemical or biological drugs. Some researchers and pharmaceutical companies are already taking this potential new class of treatments seriously and, as promising results emerge, others are expected to follow.
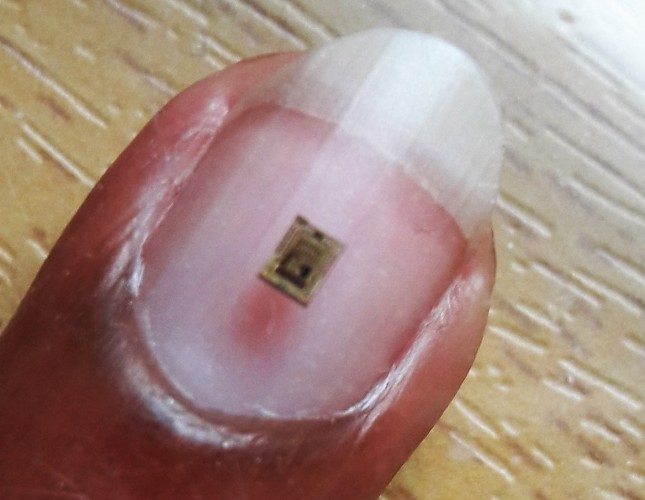
Imagine a prescription from your doctor, not for tablets but for a tiny electrical device implanted on a nerve in your neck. The device will monitor and treat your condition — whether it is diabetes, asthma, hypertension or even cancer — by modulating electrical impulses.
Pharmaceutical drugs can be highly effective, but don’t work for everyone. They tend to work systemically, often causing a variety of adverse effects, and rely on patient adherence. As a result, there are still countless chronic diseases that remain untreated or poorly treated by mainstream medicine. Enter bioelectronic medicines, a new group of therapies that work by transmitting electrical impulses along nerve fibres, rather than through molecular mechanisms. Tapping into the electrical wiring of the body, bioelectronic medicines — also called electroceuticals — could transform pharmaceutical treatment of many chronic diseases, providing an alternative or adjunct to traditional chemical or biological drugs. With technical advances and burgeoning research activity, this revolutionary approach to treating disease is starting to become a reality.
…
“Drugs are based on exercising the chemical component of our nervous systems and tend to act very globally. Electroceuticals act locally,” explains Wouter Serdijn, a bioelectronics researcher at Delft University of Technology in the Netherlands and University College London. “Moreover, contrary to drugs, electroceuticals have an instantaneous effect and their effect is reversible. It takes quite some time for drugs to [exert] their beneficial effect and, as a consequence, it takes quite some time to be able to administer the right dose.”

Source: Courtesy of Wouter Serdijn
…
It’s a tall order. “The problem with nerves is that they usually are grouped in bundles and they carry information to and from the brain, from and to the organ; often to more than one organ or to more than one part of an organ,” explains Serdijn. “So stimulation and recording nerves becomes a delicate and highly selective task.”
…
Serdijn agrees: “I think pharma perceives electroceuticals as a game changer.”



 Electrical implants of today look nothing like the first pacemaker of sixty years ago. They are much smaller now and have a much longer battery life, while being much more versatile. Small active implants now help us to relieve the symptoms of Parkinson’s disease, alleviate pain in different parts of the body and treat incontinence. According to Vasiliki Giagka, personalised electronics will soon be part of the treatment plan of patients with rheumatoid arthritis, asthma and diabetes, and patients with spinal cord injury will be able to walk again in the foreseeable future. A pipe dream? Giagka: ‘There is huge potential. I am sure there are a lot of people who will benefit from this research.’
Electrical implants of today look nothing like the first pacemaker of sixty years ago. They are much smaller now and have a much longer battery life, while being much more versatile. Small active implants now help us to relieve the symptoms of Parkinson’s disease, alleviate pain in different parts of the body and treat incontinence. According to Vasiliki Giagka, personalised electronics will soon be part of the treatment plan of patients with rheumatoid arthritis, asthma and diabetes, and patients with spinal cord injury will be able to walk again in the foreseeable future. A pipe dream? Giagka: ‘There is huge potential. I am sure there are a lot of people who will benefit from this research.’ Dr Vasiliki (Vasso) Giagka (Athens, 1984) studied Electronic and Computer Engineering at the Aristotle University in Thessaloniki, the second largest city in Greece. After graduating in 2009, she moved to London to do her PhD at University College at the Analogue and Biomedical Electronics and the Implantable Devices Groups . She participated as a post-doctoral researcher in the GlaxoSmithKline Bioelectronics Innovation Challenge. Since 2015, Giagka has been working at TU Delft as an Assistant Professor at the Bioelectronics Group, where she carries out research into new materials and approaches to the problems that come with bioelectronic medicines. She also teaches Master’s students.
Dr Vasiliki (Vasso) Giagka (Athens, 1984) studied Electronic and Computer Engineering at the Aristotle University in Thessaloniki, the second largest city in Greece. After graduating in 2009, she moved to London to do her PhD at University College at the Analogue and Biomedical Electronics and the Implantable Devices Groups . She participated as a post-doctoral researcher in the GlaxoSmithKline Bioelectronics Innovation Challenge. Since 2015, Giagka has been working at TU Delft as an Assistant Professor at the Bioelectronics Group, where she carries out research into new materials and approaches to the problems that come with bioelectronic medicines. She also teaches Master’s students.